Claim Status Tracking
“Can someone tell me what is actually going on with my claim? I get the same response again and again”
~ Neha, a loop customer
Claim will be resolved on 11 July, 24
On Time
12:22
Raise a Claim
Get Help
Current Status :
Insurer’s medical team is reviewing the documents
24th July, 24 :
Insurer has received the documents
View Detailed Timeline
TIMELINE:
Claim Registration
Completed on 05 Jul’ 24
Document Submission
Completed on 06 Jul’ 24
Review by Loop
Completed on 08 Jul’ 24
Review by Insurer
Expected date : 12 Jul’ 24
Documents received by insurer
Documents reviewed by medical team
Payment Complete
Expected date : 13 Jul’ 24
Show More
12:22
Raise a Claim
Get Help
#64846
Claim Tracking ID
On Time
Current Status :
Loop is submitting the documents to your insurer
Estimated Claim Payment Date :
24th Feb, 2023
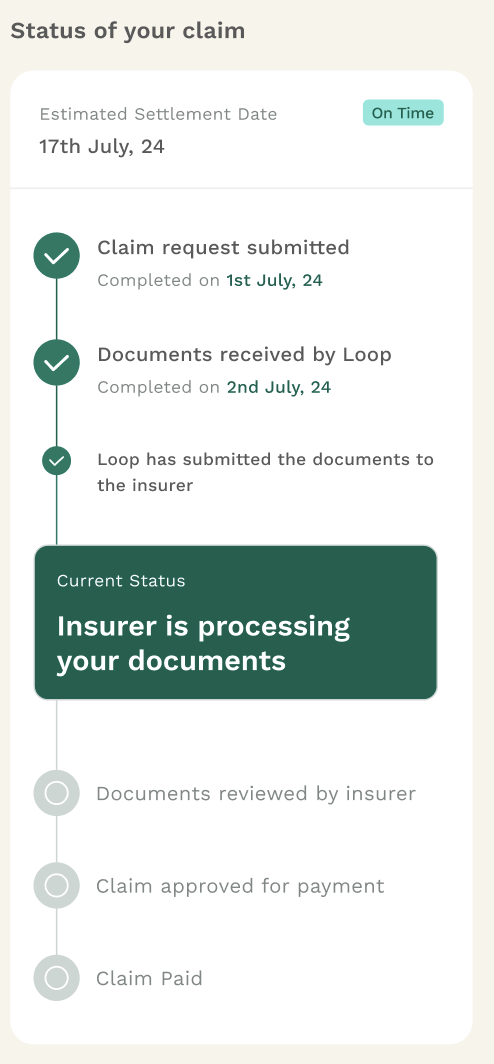
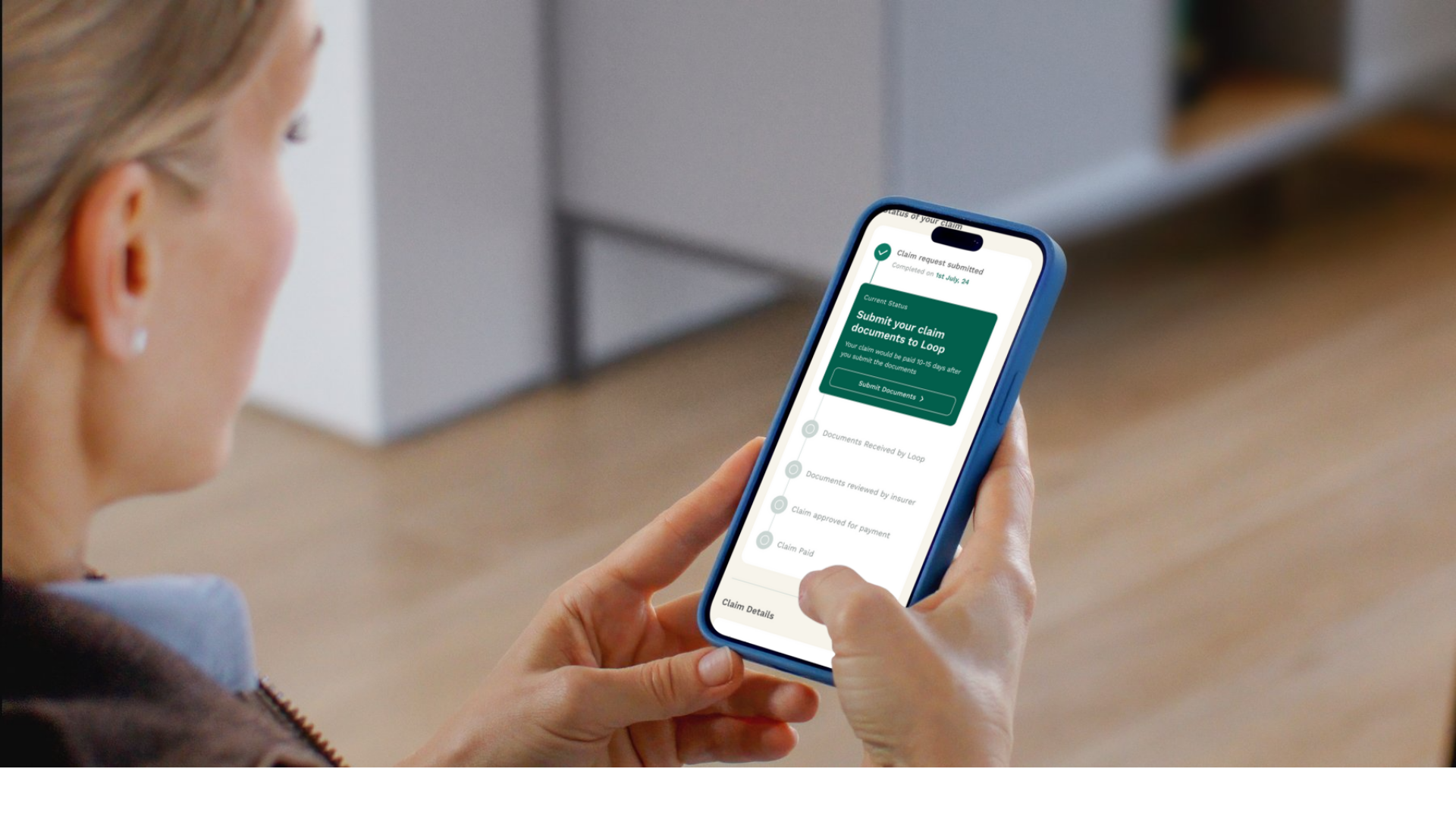
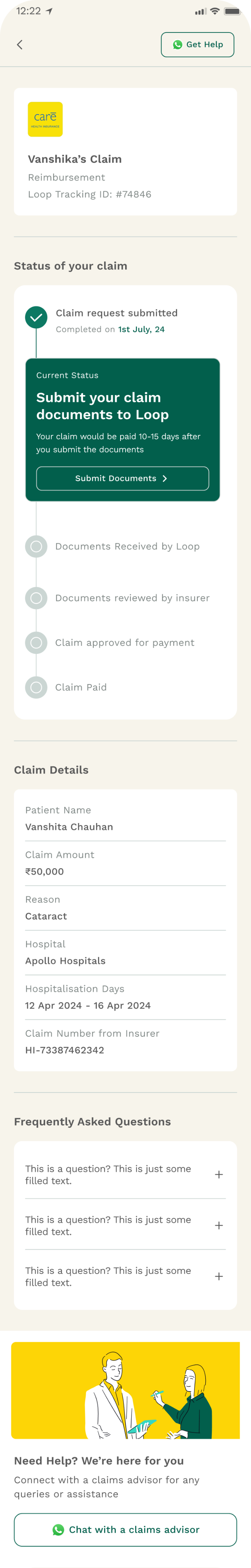
Status of your claim
Claim registered
Completed on 1st July, 24
Documents Submitted
Completed on 3rd July, 24
Loop is submitting the documents to your insurer
Takes 1-2 Days.
Claim submitted to insurer
Documents review by insurer
Takes 7-10 Days.
Claim approval
Claim payment
Takes 3-4 Days.
Claim Details
Patient Name
Anoop Agarwal
Claim Amount
₹50,000
Reason
Cataract
Hospital
Apollo Hospitals
Hospitalisation Days
12 Apr 2024 - 16 Apr 2024
Previously submitted documents
FAQs
Need Help?
Reach out instantly to Loop about any claim questions
Chat with your agent
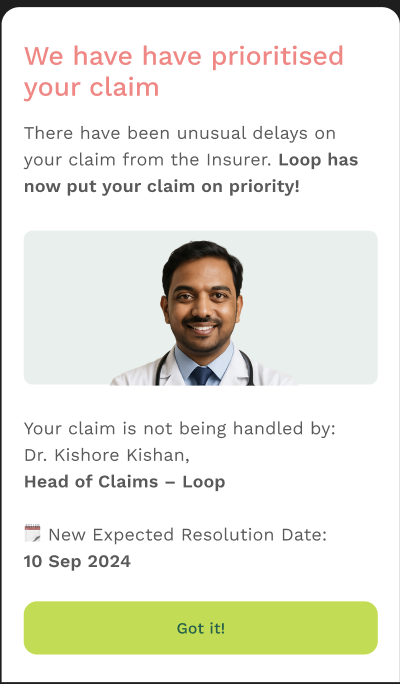
Final solution

Final solution (key components)
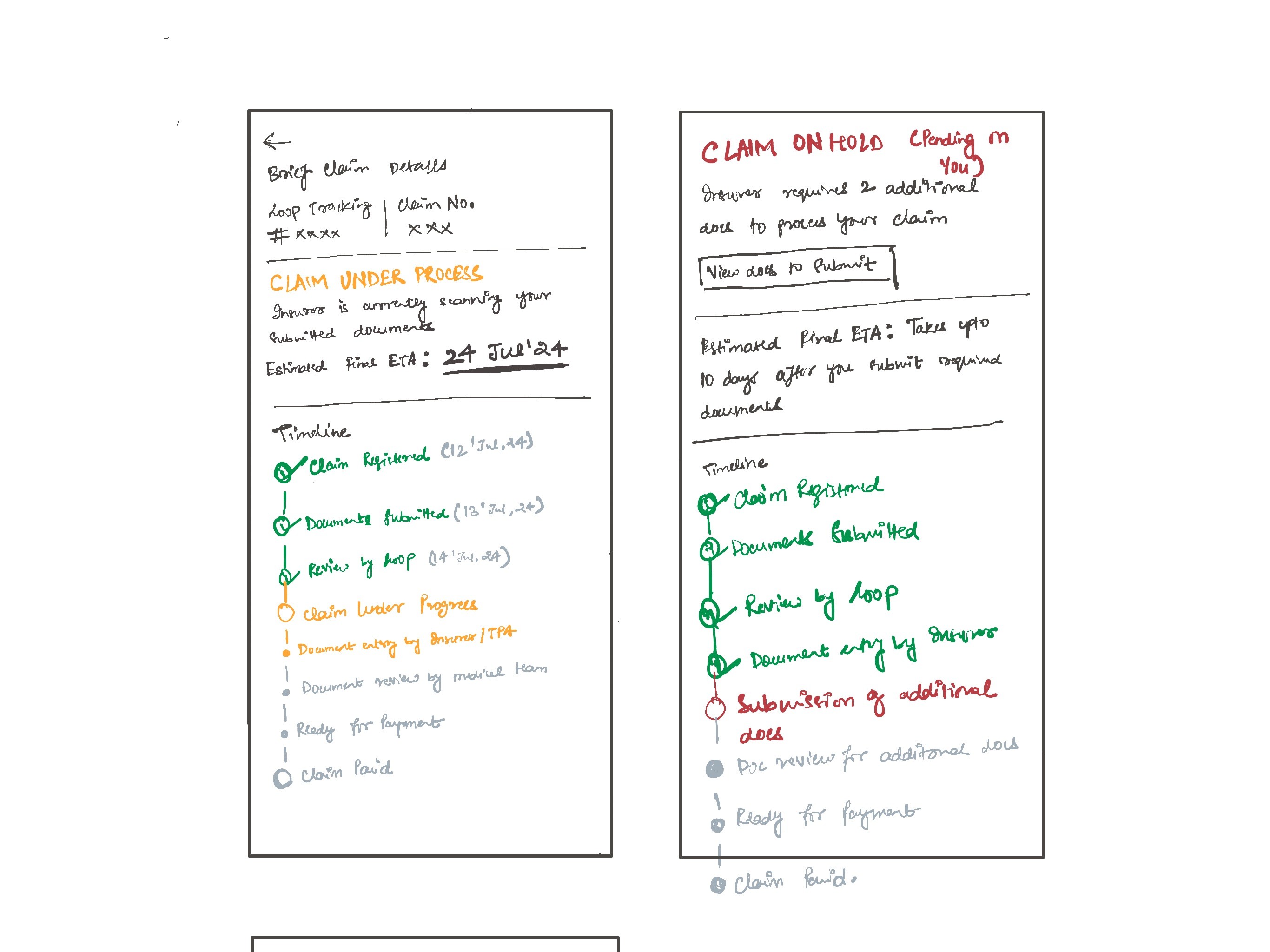
1. Timeline with Clarity and Momentum
A structured claim timeline that not only shows each stage but also:
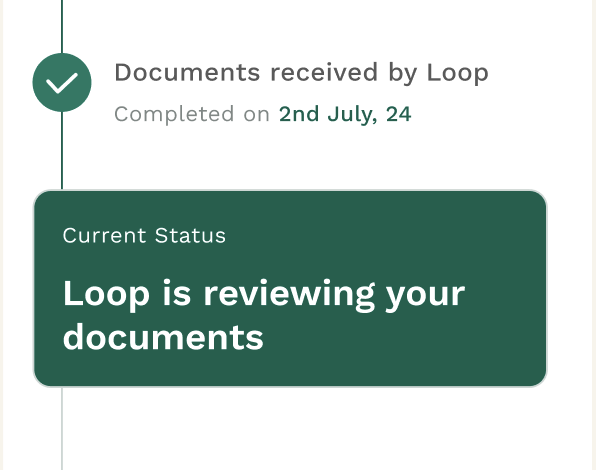
- Clearly highlights where the claim is right now
- Shows ETAs for each upcoming step, including estimated payout
- Shows sub status of claims to create a sense of progress, especially important when claim stage remains the same for a few days